- Adrenal gland
- 2023 Korean Endocrine Society Consensus Guidelines for the Diagnosis and Management of Primary Aldosteronism
-
Jeonghoon Ha, Jung Hwan Park, Kyoung Jin Kim, Jung Hee Kim, Kyong Yeun Jung, Jeongmin Lee, Jong Han Choi, Seung Hun Lee, Namki Hong, Jung Soo Lim, Byung Kwan Park, Jung-Han Kim, Kyeong Cheon Jung, Jooyoung Cho, Mi-kyung Kim, Choon Hee Chung, The Committee of Clinical Practice Guideline of Korean Endocrine Society, The Korean Adrenal Study Group of Korean Endocrine Society
-
Endocrinol Metab. 2023;38(6):597-618. Published online October 13, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1789
-
-
3,472
View
-
483
Download
-
1
Web of Science
-
1
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Primary aldosteronism (PA) is a common, yet underdiagnosed cause of secondary hypertension. It is characterized by an overproduction of aldosterone, leading to hypertension and/or hypokalemia. Despite affecting between 5.9% and 34% of patients with hypertension, PA is frequently missed due to a lack of clinical awareness and systematic screening, which can result in significant cardiovascular complications. To address this, medical societies have developed clinical practice guidelines to improve the management of hypertension and PA. The Korean Endocrine Society, drawing on a wealth of research, has formulated new guidelines for PA. A task force has been established to prepare PA guidelines, which encompass epidemiology, pathophysiology, clinical presentation, diagnosis, treatment, and follow-up care. The Korean clinical guidelines for PA aim to deliver an evidence-based protocol for PA diagnosis, treatment, and patient monitoring. These guidelines are anticipated to ease the burden of this potentially curable condition.
-
Citations
Citations to this article as recorded by  - Correlation of Histopathologic Subtypes of Primary Aldosteronism with Clinical Phenotypes and Postsurgical Outcomes
Chang Ho Ahn, You-Bin Lee, Jae Hyeon Kim, Young Lyun Oh, Jung Hee Kim, Kyeong Cheon Jung
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef
- Thyroid
- Exploring the Association between Thyroid Function and Frailty: Insights from Representative Korean Data
-
Youn-Ju Lee, Min-Hee Kim, Dong-Jun Lim, Jung-Min Lee, Sang Ah Chang, Jeongmin Lee
-
Endocrinol Metab. 2023;38(6):729-738. Published online November 2, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1769
-
-
1,106
View
-
73
Download
-
1
Web of Science
-
1
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
This study investigates the association between thyroid function and frailty in the old patients using representative data.
Methods
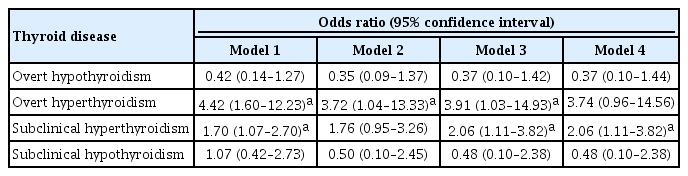
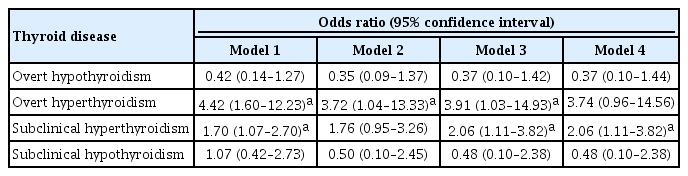
The study was conducted using data from the Korea National Health and Nutrition Examination Survey conducted from 2013 to 2015. The study population included 2,416 participants aged 50 years and older with available thyroid function test data. Frailty assessment was performed using the Fried frailty phenotype. The prevalence of frailty was analyzed across different thyroid diseases and thyroid function parameters.
Results
The significant association between thyroid dysfunction and frailty was observed in overt hyperthyroidism and subclinical hyperthyroidism. After adjusting for various factors, the association between thyroid dysfunction and frailty remained significant. On the other hand, overt hypothyroidism did not show a significant association with frailty in the adjusted analysis. For individuals with overt hyperthyroidism and subclinical hyperthyroidism, higher levels of free thyroxine (FT4) were significantly associated with an increased risk of frailty (aOR >999; 95% CI, >999 to 999). Among individuals with overt hypothyroidism, lower level of FT4 levels and high thyrotropin (TSH) levels showed a significant association with frailty risk (FT4: aOR, <0.01; TSH: aOR, 999). In participants with subclinical hypothyroidism, there were no significant associations between parameters for thyroid and frailty risk.
Conclusion
These findings suggest that thyroid dysfunction, particularly overt hyperthyroidism and subclinical hyperthyroidism, may be associated with an increased risk of frailty in the old patients.
-
Citations
Citations to this article as recorded by  - Associations of thyroid feedback quantile-based index with diabetes in euthyroid adults in the United States and China
Heng Wan, Genfeng Yu, Yajun He, Siyang Liu, Xingying Chen, Yuqi Jiang, Hualin Duan, Xu Lin, Lan Liu, Jie Shen
Annals of Medicine.2024;[Epub] CrossRef
- Thyroid
- Beyond Acute COVID-19: Investigating the Incidence of Subacute Thyroiditis in Long COVID-19 in Korea
-
Jeongmin Lee, Gi Hyeon Seo, Keeho Song
-
Endocrinol Metab. 2023;38(4):455-461. Published online August 8, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1711
-
-
2,635
View
-
181
Download
-
3
Web of Science
-
4
Crossref
-
 Abstract Abstract
 PDF PDF PubReader PubReader  ePub ePub
- Background
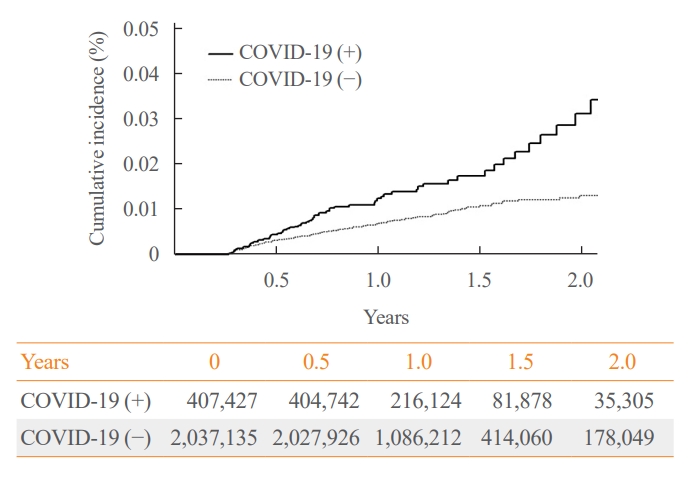
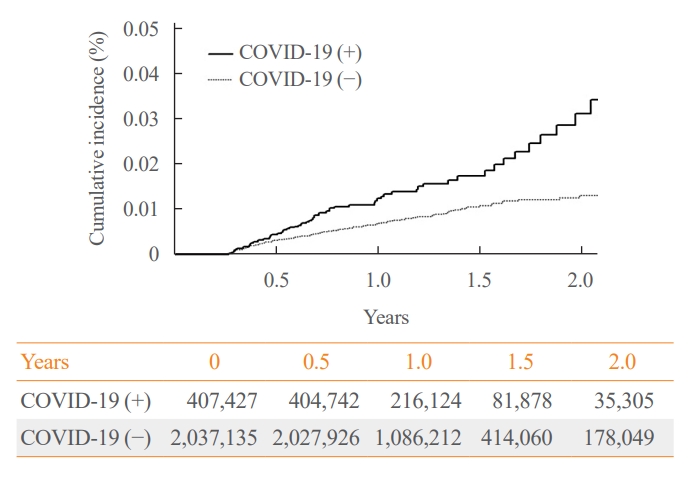
The correlation between acute coronavirus disease 2019 (COVID-19) and subacute thyroiditis (SAT) has not been clearly investigated in “long COVID” patients. We aimed to investigate the incidence of SAT during convalescence and after the acute phase of COVID-19, comparing with that of the general population.
Methods
Data from a total of 422,779 COVID-19 patients and a control group of 2,113,895 individuals were analyzed. The index date was defined as the date 3 months after confirmation of COVID-19. The incidence rate (IR) of SAT and hazard ratios (HRs) were calculated per 100,000 persons. Subgroup analysis included analysis of HRs 90–179 and 180 days post-COVID-19 diagnosis; and additional analysis was conducted according to hospitalization status, sex, and age group.
Results
The IR of SAT was 17.28 per 100,000 persons (95% confidence interval [CI], 12.56 to 23.20) in the COVID-19 group and 8.63 (95% CI, 6.37 to 11.45) in the control group. The HR of COVID-19 patients was 1.76 (95% CI, 1.01 to 3.06; P=0.045). The HR of SAT was 1.39 (95% CI, 0.82 to 2.34; P=0.220) up to 6 months after the index date and 2.30 (95% CI, 1.60 to 3.30; P<0.001) beyond 6 months. The HR for SAT among COVID-19 patients was 2.00 (95% CI, 1.41 to 2.83) in hospitalized patients and 1.76 (95% CI, 1.01 to 3.06) in non-hospitalized patients compared to the control group. The IR of SAT was 27.09 (95% CI, 20.04 to 35.82) for females and 6.47 (95% CI, 3.34 to 11.30) for males. In the 19 to 64 age group, the IR of SAT was 18.19 (95% CI, 13.70 to 23.67), while the IR was 9.18 (95% CI, 7.72 to 10.84) in the 65 to 69 age group.
Conclusion
SAT could be a potential long-term complication of COVID-19. Long-term surveillance for thyroid dysfunction is needed especially in hospitalized, female and young-aged subjects.
-
Citations
Citations to this article as recorded by  - Thyroid dysfunction in COVID-19
David Tak Wai Lui, Chi Ho Lee, Yu Cho Woo, Ivan Fan Ngai Hung, Karen Siu Ling Lam
Nature Reviews Endocrinology.2024;[Epub] CrossRef - Subacute Thyroiditis in the Time of COVID-19
Hwa Young Ahn
Endocrinology and Metabolism.2024; 39(1): 186. CrossRef - Occult endocrine disorders newly diagnosed in patients with post-COVID-19 symptoms
Yasuhiro Nakano, Naruhiko Sunada, Kazuki Tokumasu, Hiroyuki Honda, Yuki Otsuka, Yasue Sakurada, Yui Matsuda, Toru Hasegawa, Daisuke Omura, Kanako Ochi, Miho Yasuda, Hideharu Hagiya, Keigo Ueda, Fumio Otsuka
Scientific Reports.2024;[Epub] CrossRef - rRisk of incident thyroid dysfunction in the post-acute phase of COVID-19: a population-based cohort study in Hong Kong
David Tak Wai Lui, Xi Xiong, Ching‐Lung Cheung, Francisco Tsz Tsun Lai, Xue Li, Eric Yuk Fai Wan, Celine Sze Ling Chui, Esther Wai Yin Chan, Franco Wing Tak Cheng, Lanlan Li, Matthew Shing Hin Chung, Chi Ho Lee, Yu Cho Woo, Kathryn Choon Beng Tan, Carlos
Endocrine Practice.2024;[Epub] CrossRef
- Thyroid
- The Early Changes in Thyroid-Stimulating Immunoglobulin Bioassay over Anti-Thyroid Drug Treatment Could Predict Prognosis of Graves’ Disease
-
Jin Yu, Han-Sang Baek, Chaiho Jeong, Kwanhoon Jo, Jeongmin Lee, Jeonghoon Ha, Min Hee Kim, Jungmin Lee, Dong-Jun Lim
-
Endocrinol Metab. 2023;38(3):338-346. Published online June 9, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1664
-
-
1,746
View
-
102
Download
-
1
Web of Science
-
2
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
To determine whether baseline thyroid-stimulating immunoglobulin (TSI) bioassay or its early response upon treatment with an anti-thyroid drug (ATD) can predict prognosis of Graves’ disease (GD) in real-world practice.
Methods
This retrospective study enrolled GD patients who had previous ATD treatment with TSI bioassay checked at baseline and at follow-up from April 2010 to November 2019 in one referral hospital. The study population were divided into two groups: patients who experienced relapse or continued ATD (relapse/persistence), and patients who experienced no relapse after ATD discontinuation (remission). The slope and area under the curve at 1st year (AUC1yr) of thyroid-stimulating hormone receptor antibodies including TSI bioassay and thyrotropin-binding inhibitory immunoglobulin (TBII) were calculated as differences between baseline and second values divided by time duration (year).
Results
Among enrolled 156 study subjects, 74 (47.4%) had relapse/persistence. Baseline TSI bioassay values did not show significant differences between the two groups. However, the relapse/persistence group showed less decremental TSI bioassay in response to ATD than the remission group (–84.7 [TSI slope, –198.2 to 8.2] vs. –120.1 [TSI slope, –204.4 to –45.9], P=0.026), whereas the TBII slope was not significantly different between the two groups. The relapse/persistence group showed higher AUC1yr of TSI bioassay and TBII in the 1st year during ATD treatment than the remission group (AUC1yr for TSI bioassay, P=0.0125; AUC1yr for TBII, P=0.001).
Conclusion
Early changes in TSI bioassay can better predict prognosis of GD than TBII. Measurement of TSI bioassay at beginning and follow-up could help predict GD prognosis.
-
Citations
Citations to this article as recorded by  - Enhanced predictive validity of integrative models for refractory hyperthyroidism considering baseline and early therapy characteristics: a prospective cohort study
Xinpan Wang, Tiantian Li, Yue Li, Qiuyi Wang, Yun Cai, Zhixiao Wang, Yun Shi, Tao Yang, Xuqin Zheng
Journal of Translational Medicine.2024;[Epub] CrossRef - Long-term effect of thyrotropin-binding inhibitor immunoglobulin on atrial fibrillation in euthyroid patients
Jung-Chi Hsu, Kang-Chih Fan, Ting-Chuan Wang, Shu-Lin Chuang, Ying-Ting Chao, Ting-Tse Lin, Kuan-Chih Huang, Lian-Yu Lin, Lung-Chun Lin
Endocrine Practice.2024;[Epub] CrossRef
- Calcium & bone metabolism
- Persistence with Denosumab in Male Osteoporosis Patients: A Real-World, Non-Interventional Multicenter Study
-
Chaiho Jeong, Jeongmin Lee, Jinyoung Kim, Jeonghoon Ha, Kwanhoon Jo, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Tae-Seo Sohn, Ki-Ho Song, Moo Il Kang, Ki-Hyun Baek
-
Endocrinol Metab. 2023;38(2):260-268. Published online April 27, 2023
-
DOI: https://doi.org/10.3803/EnM.2023.1663
-
-
1,762
View
-
109
Download
-
1
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
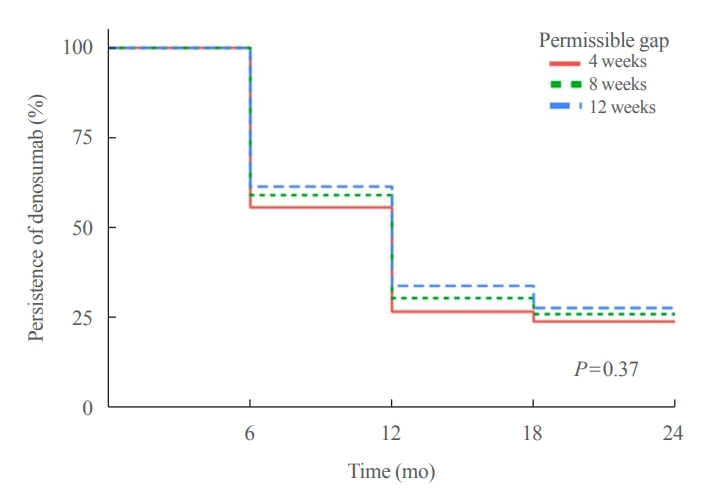
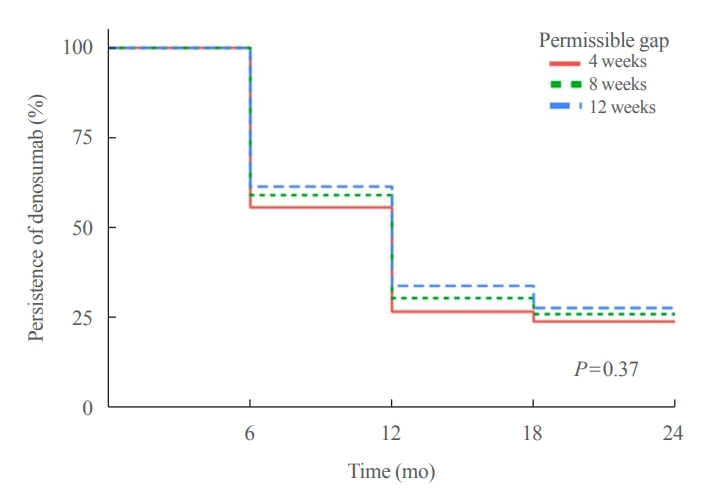
- Background
Persistence with denosumab in male patients has not been adequately investigated, although poor denosumab persistence is associated with a significant risk of rebound vertebral fractures.
Methods
We retrospectively evaluated 294 Korean male osteoporosis patients treated with denosumab at three medical centers and examined their persistence with four doses of denosumab injection over 24 months of treatment. Persistence was defined as the extent to which a patient adhered to denosumab treatment in terms of the prescribed interval and dose, with a permissible gap of 8 weeks. For patients who missed their scheduled treatment appointment(s) during the follow-up period (i.e., no-shows), Cox proportional regression analysis was conducted to explore the factors associated with poor adherence. Several factors were considered, such as age, prior anti-osteoporotic drug use, the treatment provider’s medical specialty, the proximity to the medical center, and financial burdens of treatment.
Results
Out of 294 male patients, 77 (26.2%) completed all four sequential rounds of the denosumab treatment. Out of 217 patients who did not complete the denosumab treatment, 138 (63.6%) missed the scheduled treatment(s). Missing treatment was significantly associated with age (odds ratio [OR], 1.03), prior bisphosphonate use (OR, 0.76), and prescription by non-endocrinologists (OR, 2.24). Denosumab was stopped in 44 (20.3%) patients due to medical errors, in 24 (11.1%) patients due to a T-score improvement over –2.5, and in five (2.3%) patients due to expected dental procedures.
Conclusion
Our study showed that only one-fourth of Korean male osteoporosis patients were fully adherent to 24 months of denosumab treatment.
-
Citations
Citations to this article as recorded by  - Denosumab
Reactions Weekly.2023; 1963(1): 206. CrossRef
- Thyroid
- Quality of Life of Survivors of Thyroid Cancer Is Not Inferior to That in Subjects without Cancer: Long-Term after Over 5 Years
-
Jeongmin Lee, Youn-Ju Lee, Dong-Jun Lim, Jung-Min Lee, Sang-Ah Chang, Min-Hee Kim
-
Endocrinol Metab. 2022;37(4):664-673. Published online August 29, 2022
-
DOI: https://doi.org/10.3803/EnM.2022.1499
-
-
3,172
View
-
184
Download
-
2
Web of Science
-
3
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
Patients with thyroid cancer undergo less extensive surgery and additional therapies compared to those with other cancers. We aimed to compare the quality of life (QoL) between patients with thyroid cancer and healthy subjects using representative data from Korea. Differences in QoL of thyroid cancer survivors according to the duration after cancer diagnosis was also evaluated.
Methods
This population-based cohort study included 50,278 subjects who participated in the Korea National Health and Nutrition Examination Survey between 2007 and 2017. QoL was compared between patients with thyroid cancer and healthy subjects using self-reported data from the EuroQoL (EQ)-5 dimension (5D) and EQ-visual analog scale (VAS). Propensity score matching was used to match thyroid cancer survivors to healthy subjects (1:5 matching).
Results
Linear regression with univariate analysis showed that the presence of thyroid cancer was positively correlated with better EQ-5D index scores (β-coefficient=0.010, p=0.046). After adjusting for multiple covariables, statistical significance was maintained. EQ-VAS fails to demonstrate any significant correlation. Among the EQ-5D categories, patients with thyroid cancer showed better self-care than healthy subjects. Thyroid cancer duration did not correlate with the EQ-5D index score. In subgroup analyses, compared to patients with thyroid cancer duration of <5 years, no significant difference was observed in the correlation between the EQ-5D index score and survival duration in those with thyroid cancer duration of 5 to 9 years and ≥10 years.
Conclusion
Using a large-scale nationwide population-based database, our study demonstrated better QoL, especially in terms of self-care, among thyroid cancer survivors than among healthy subjects without cancer.
-
Citations
Citations to this article as recorded by  - Quality of Life Considerations in Patients Treated for Differentiated Thyroid Cancer
Jie Liu
Clinical Thyroidology.2023; 35(4): 160. CrossRef - The psychosocial impact of thyroid cancer
Parker Haymart, Nina Jackson Levin, Megan R. Haymart
Current Opinion in Endocrinology, Diabetes & Obesity.2023; 30(5): 252. CrossRef - Longitudinal Changes in Quality of Life Before and After Thyroidectomy in Patients With Differentiated Thyroid Cancer
Byung Hun Kim, Soo Rack Ryu, Jin Won Lee, Chang Myeon Song, Yong Bae Ji, Seok Hyun Cho, Seung Hwan Lee, Kyung Tae
The Journal of Clinical Endocrinology & Metabolism.2023;[Epub] CrossRef
|